Why Use Antibiotics Over and Over Again to Heal Wounds
Abstract
We have all experienced a wound, a local injury to the skin, at some point in our lives. Most frequently, wounds heal completely and a scab is the only sign of the injury. Except for the initial pain and bleeding, we might not pay much attention to the procedure past which the wound repairs or the possible complications that could ascend. The process of wound healing involves a well-coordinated series of steps involving many cells, tissues, and chemicals in the torso. Interruptions to the wound healing process, ofttimes caused by the presence of bacteria, lead to major disturbances and delays in wound repair. Farther, some forms of bacteria can be resistant to antibiotics, making information technology difficult to treat infected wounds. In this commodity, we discuss the stages of wound healing, explain how bacteria can filibuster this process, and describe simple steps that you tin prefer to prevent wound infections.
Introduction
Ouch! Do yous remember the terminal time you fell on the playground and injured your pare? Or accidently slashed your fingertip while using a knife? Maybe it was not very long ago. You might likewise remember what happened after that. The injury might accept oozed some blood, which stopped soon after to reveal reddish, damaged skin. If the injury was deep, you may have visited the doctor. The doctor would have cleaned the damaged skin and covered it with a bandage. Over the next few days, you may have observed the injured pare modify colors from brilliant red to bluish-black, and finally, the injury would have been replaced with fresh skin. After the damaged skin has healed, you may run into a flesh-colored scar at the location of the injury. If this sounds familiar, it means that your adventitious injury resulted in what is chosen a wound, which was followed by the normal steps of recovery known as wound healing. It is likely that your wound eventually healed without any bug.
Wounds
The peel is the largest organ of the torso and information technology acts as a protective covering shielding the body from the outer surroundings. The epidermis is the outermost layer of the skin, consisting of cells known every bit keratinocytes. The eye layer, or dermis , contains another type of skin jail cell known as fibroblasts, and claret vessels that behave blood to and from the skin. The dermis also has tissue fibers that provide support to cells within the skin.
A break in these layers of the peel, often resulting from a accident or cut, tin can crusade a disturbance in the pare's structure and function, and is known as a wound. Superficial wounds are injuries to only the epidermis. Deep wounds extend all the way into the dermis, causing greater damage to skin cells and tissue fibers, resulting in a gap in the pare. In deep wounds, the claret vessels too become damaged, leading to leaks, which is why these wounds bleed. So, what happens afterwards we get hurt and how does the torso answer to a wound?
Wound Healing
After an injury, the torso starts repairing damaged peel through the process of wound healing, which involves a set of iv well-coordinated steps (Effigy ane) [1]. The first footstep involves stopping the blood flow past formation of a blood clot at the wound, and this happens almost immediately afterwards an injury. To form a clot, blood components interact to class a loose plug of protein strands and blood cells at the wound site. Next, large numbers of immune cells get in at the wound site through claret vessels, releasing chemicals that outset to build new tissue in the wound. In the tertiary phase, the wound is gradually filled with new peel tissue that replaces the gap created by the injury. This works somewhat like edifice blocks, in which different types of skin proteins human action as a solid, sticky surface on which many layers of skin cells can adhere and grow. In the concluding stage of wound healing, this new skin tissue gets strengthened and completely fills the wound. This step replaces the damaged tissue with scar tissue that closely resembles normal peel. This completes the process of wound healing. The entire procedure of wound healing starts immediately after injury and ordinarily takes a few weeks. Notwithstanding, in certain situations, wounds practice not follow this coordinated repair procedure, taking a long time to heal or not healing at all. Why do some wounds neglect to heal properly?
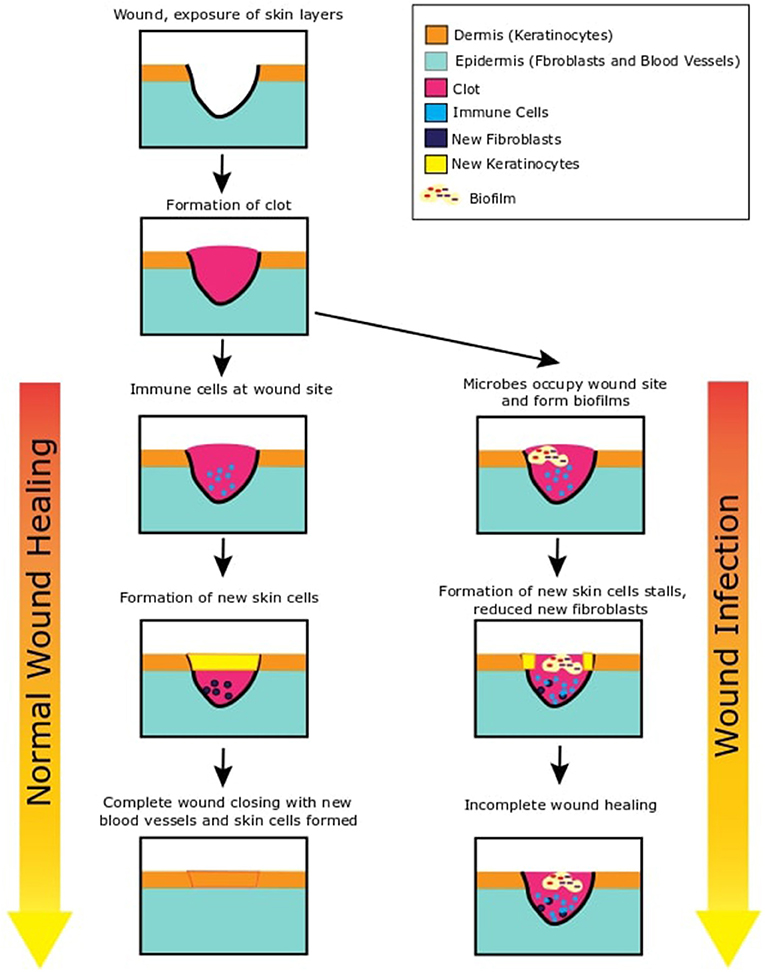
- Effigy 1 - This figure shows ii possible outcomes after the skin is wounded.
- On the left side of this figure, we see what happens when wounds heal normally. After the skin is wounded, inner layers of the skin are exposed. A claret clot is immediately formed to stop loss of blood. Immune cells migrate to the wound site and release chemicals. These chemical signal the skin layers (epidermis and dermis) to abound new skin cells that move to make full in the gap of the wound. At the terminate, the newly formed skin tissue strengthens and closes the wound to restore the skin integrity. On the right side of this effigy, we can encounter what is likely to happen in the case of an infection. Bacteria occupy the open up wound and start growing and increasing in number. They course biofilms in the wound. They as well secrete chemicals to inhibit any protective systems of our skin. Every bit the immune cells cannot articulate the bacteria, the infection continues and new skin cell formation is paused. This can remain stalled and result in incomplete wound healing.
Wound Infections
One of the main reasons that wounds may fail to heal properly is the presence and growth of microbes , which are very tiny forms of life, in the wound. Microbes are tiny organisms that cannot exist seen with the naked heart. While many microbes are beneficial to us, certain harmful microbes tin can make united states of america ill, and this is known every bit an infection . When harmful microbes live and reproduce in a wound, it leads to a wound infection [2]. Wound infections slow downwardly and sometimes prevent the process of healing. Bacteria are the microbes that most often cause wound infections, and a wound can commonly exist infected with more than than 1 type of leaner. Only how practice leaner enter wounds in the offset identify? One possibility is through an object or material that has bacteria on it, like mayhap an unclean pocketknife or soil from the playground. Another possibility is that bacteria from the surrounding air can settle on an open wound surface. In fact, this is why doctors often cover wounds with bandages—to prevent exposure to microorganisms in the air. The peel does have defense strategies to remove leaner that settle on the wound, and frequently bacteria are killed and wound healing resumes. Nevertheless, conditions, such equally improper cleaning of the wound, poor full general health, erstwhile age, or diseases, such as diabetes can weaken the skin's protective systems, increasing the chances of wound infections. These situations may lead to non-healing wounds, which tin can increase pain, discomfort, and time and coin spent in the hospital or on treatment. In extreme cases, spread of the infection tin can also require the doctors to cut off the infected limb!
A Closer Look at Bacteria in Wounds
One time bacteria enter or settle on damaged skin, the wound provides the necessary nutrients for them to increment in number and spread the infection. In these ideal conditions, private bacteria grow to form big-scale bacterial communities known every bit biofilms (Figure 1) [three]. Biofilms consist of large numbers of bacteria amassed together to form dumbo, mat-like structures that cover the entire surface of the wound [4]. Biofilm bacteria are held together by a mesh of protein and sugars, resembling a glue, oft made by the leaner themselves. This mesh not only strengthens the biofilm construction from within but as well serves equally a protective covering for the bacteria, surrounding the unabridged biofilm. When bacteria grow within the wound, they produce small chemicals that are used every bit signals to communicate with other leaner every bit well as to touch immune cells and blood vessels of the host they infect. Allowed cells can respond to these signals in an attempt to impale the bacteria and limit spread of the infection. However, the high density of leaner and the toxic chemicals the leaner produce can reduce the ability of immune cells to impale the leaner, making the body unable to remove the biofilm. This results in further growth and spread of the biofilm, which in turn further complicates and delays wound healing.
The removal of wound biofilms requires medical intervention, usually in the form of treatment with antibiotics . Antibiotics are applied as ointments, bandages or by flowing a solution across the wound. Wound biofilms frequently require multiple applications of antibiotics, over several days. Fifty-fifty if the proper handling is given, wound biofilms can persist and result in a wound that fails to heal [4].
Why is Information technology Difficult to Treat Wound Biofilms?
Biofilm bacterial communities can sometimes survive handling with antibiotics. Ane of the reasons for this is the density of bacteria in the biofilm, reminding us of the quote, "united we stand up, divided nosotros fall." Concentrations of antibiotics that piece of work against pocket-size numbers of bacteria may not be enough to kill or prevent the growth of large numbers of biofilm bacteria. These bacteria are also embedded in a mesh of proteins and sugars that forms a roofing effectually the biofilm. This mesh can act every bit a baby-sit, slowing down the entry of antibiotics into the inner parts of the biofilm and protecting the bacteria at the center of the biofilm. Bacteria in biofilms also produce chemicals that tin can pause down sure antibiotics. Finally, biofilm bacteria also have the ability to slow downward their growth and reduce their nutrient consumption but withal remain live in a dormant land, with low action. This tricks the antibiotics, because some antibiotics target only growing bacterial cells. These fallow bacteria can survive antibody treatment and begin to abound again when the treatment stops.
What Can Be Done to Help Wounds Heal?
Given the difficulty of successfully treating wound biofilm leaner with antibiotics, medical doctors and scientific researchers are actively looking for new approaches to eliminate wound biofilms. New methods include applying plant-based extracts to kill microbes, using good leaner (probiotics) to compete with harmful wound bacteria, exposing the wound to bluish low-cal or vacuum forces, or using a combination of these treatments [five]. In any instance, the best strategy would be to forestall wound infections, peculiarly among people who are at risk for non-healing wounds. For this, as a young citizen-scientist, the first steps you tin take are removing any foreign material from the wound, applying antibody ointment, and loosely wrapping the wound in a protective bandage, after which a doctor can evaluate the injury (Figure ii). And then, the next fourth dimension you witness a fall on the playground, you have all the information you demand to help yourself and those around you lot understand wounds, how they heal, what happens when they get infected, and why nosotros should attempt to prevent infections. Ah-ha to that!
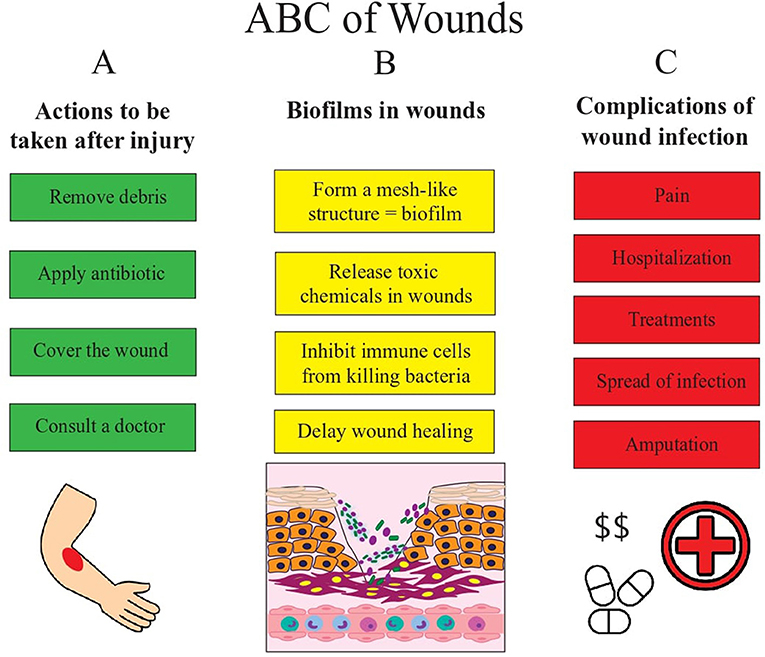
- Effigy 2 - This figures shows us the basic ABCs of wounds.
- (A) Afterwards the skin is wounded, proper intendance and handling is necessary to prevent infection and promote normal wound healing. Wounds demand to be cleaned and antibiotics should be applied to prevent infection. In cases of astringent wounds or when in uncertainty on how to proceed, pay a visit to the md. If not treated properly, wounds can get infected. (B) Bacteria tin enter wounds and form biofilms. They release chemicals that prevent immune cells from killing these bacteria and this delays wound healing. When the number of leaner in the wound increase even more and the infection becomes astringent, it can atomic number 82 to complications. (C) The non-healing wound tin crusade a lot of pain and require you to stay at the hospital to get handling. Infections tin can besides spread to other parts of the body. In some serious cases where even treatment is not helping remove the infection, the doctors may take to cut off the limb or part of the skin where the infection occurs.
Glossary
Epidermis: ↑ The outer layer of your pare. When you look at your pare, you meet the topmost office of the epidermis, consisting of expressionless cells. At the bottom of the epidermis, new cells are fabricated and they gradually move upwards to the surface and continuously replace older cells.
Dermis: ↑ The layer of the skin below the epidermis consisting of blood vessels, pilus follicles, sweat glands, oil glands, nerve endings.
Immune Cells: ↑ Cells that defend the body against invaders, such every bit microbes.
Microbes: ↑ Microscopic forms of life, such as bacteria, viruses, fungi, and protozoa, some of which can cause infections in humans.
Infection: ↑ When harmful microbes enter the torso, in a location where they do not belong, information technology is called an infection. These microbes are harmful to the body in infections.
Biofilm: ↑ A customs of bacteria living together within a meshed covering of proteins they secrete.
Antibiotic: ↑ A medicine that kills or prevents the growth of microbes.
Disharmonize of Involvement
The authors declare that the research was conducted in the absence of whatever commercial or financial relationships that could be construed as a potential conflict of involvement.
References
[1] ↑ Gurtner, G. C., Werner, S., Barrandon, Y., and Longaker, M. T. 2008. Wound repair and regeneration. Nature 453:314–21. doi: 10.1038/nature07039
[2] ↑ Bowler, P. G., Duerden, B. I., and Armstrong, D. G. 2001. Wound microbiology and associated approaches to wound management. Clin. Microbiol. Rev. fourteen:244–69. doi: x.1128/CMR.fourteen.2.244-269.2001
[3] ↑ Costerton, J. W., Lewandowski, Z., Caldwell, D. E., Korber, D. R., and Lappin-Scott, H. M. 1995. Microbial biofilms. Annu. Rev. Microbiol. 49:711–45.
[4] ↑ Zhao, G., Usui, Chiliad. 50., Lippman, S. I., James, G. A., Stewart, P. S., Fleckman, P., et al. 2013. Biofilms and inflammation in chronic wounds. Adv. Wound Care (New Rochelle) ii:389–99. doi: 10.1089/wound.2012.0381
[5] ↑ Kadam, S., Shai, S., Shahane A., and Kaushik, 1000. Due south. 2019. Recent advances in not-conventional antimicrobial approaches for chronic wound biofilms: have we plant the 'Chink in the Armor'? Biomedicines 7:35. doi: 10.3390/biomedicines7020035
Source: https://www.frontiersin.org/articles/490548
0 Response to "Why Use Antibiotics Over and Over Again to Heal Wounds"
Postar um comentário